
ANGIOGRAPHYANDINTERVENTION.COM
Ovarian Vein Embolization (OVE)

Ovarian vein embolization (OVE) is a minimally invasive procedure performed by an interventional radiologist to treat pelvic congestion syndrome (PCS). PCS is a condition characterized by chronic pelvic pain and discomfort in women, which is thought to be caused by the dilation and reflux of the ovarian veins, leading to venous congestion and inflammation of the pelvic organs.
Patients with PCS may experience a variety of symptoms, including pelvic pain that worsens with prolonged standing or sitting, heaviness or pressure in the pelvis, and pain during sexual intercourse. Other symptoms may include irregular menstrual cycles, abdominal bloating, and urinary symptoms such as frequency and urgency.
Angiographically, the tortuous varicose veins are demonstrated in the pelvic cavity, where contrast congests or pools within this region as the valves are dysfunctional and fail to regulate normal venous return towards the heart. A majority of PCS presentations are caused by dilation and reflux of the left ovarian vein, followed by the right ovarian vein, and unilateral or bilateral internal iliac veins.
By blocking the ovarian vein(s) and other contributing veins with embolic materials, the reflux of blood is stopped, reducing the congestion and inflammation of the pelvic organs that causes the symptoms of PCS. The embolic materials create a barrier that prevents blood from flowing through the affected vein(s) and diverts it to other healthy veins.
A&I Protocol
OVE can be performed by either a jugular approach or femoral approach. Both approaches are detailed here:
Jugular Approach:
-
Seldinger technique is used to gain access into the right internal jugular vein.
-
A 5 French (F) sheath is inserted into the right internal jugular vein over an 0.035" guidewire.
-
A 5 F Multi-purpose catheter is navigated down the superior vena cava (SVC), and inferior vena cava (IVC) towards the level of the left renal vein at approximately the second lumbar vertebrae (L2).
-
Under fluoroscopy, small amounts of contrast is injected to visualize the origin of the left ovarian vein and accessed using the 5 F catheter and guidewire.
-
Different guidewires can be used to try and access the left renal vein and left ovarian vein if a standard 0.035" is not compatible (e.g. 0.035" glide-wire).
-
Under fluoroscopy, the patient is instructed to perform a Valsalva maneuver (forceful expiration under a closed airway) while injecting contrast through the 5 F catheter to highlight the left ovarian vein dilatation and the congestion of pelvic varicose veins.
-
The ovarian vein/s diameters are measured on the angiography machine and the embolization coils are upsized by 10%.
-
Deployment of embolization coils are performed from the distal to proximal direction. Sclerotherapy drugs which contain sodium tetradecyl sulfate can be used between coils to assist with treating the varicose veins.
-
Contrast injections under fluoroscopy is used to check that the left ovarian vein (single or multiple branches) are embolized and prevent contrast from travelling down towards to the pelvis. It is important to also allow some time to pass before checking to allow the coils to expand.
-
Following embolization of the left ovarian vein, the right renal vein and right ovarian vein are checked for contribution to the PCS. If PCS is demonstrated then embolization coils (and sclerosants) are used to block the right ovarian vein.
-
Following this, the left and right internal iliac veins are imaged under fluoroscopy, contrast injection, and Valsalva maneuver. If dilatation and reflux is demonstrated, then embolization coils are deployed to treat these veins.
-
The vascular devices are removed post-procedure, pressure is applied on the neck region, and the angiography table can be placed in reverse-Trendelenburg position.
Femoral Approach:
-
Seldinger technique is used to gain access into the right common femoral vein.
-
A 5 French (F) sheath is inserted into the right common femoral vein over an 0.035" guidewire.
-
A 5 F Hockey-stick catheter is navigated up the IVC towards the level of the left renal vein at approximately the second lumbar vertebrae (L2).
-
Under fluoroscopy, small amounts of contrast is injected to visualize the origin of the left ovarian vein and accessed using the 5 F catheter and guidewire.
-
Different guidewires can be used to try and access the left renal vein and left ovarian vein if a standard 0.035" is not compatible (e.g. 0.035" glide-wire).
-
Under fluoroscopy, the patient is instructed to perform a Valsalva maneuver (forceful expiration under a closed airway) while injecting contrast through the 5 F catheter to highlight the left ovarian vein dilatation and the congestion of pelvic varicose veins.
-
The ovarian vein/s diameters are measured on the angiography machine and the embolization coils are upsized by 10%.
-
Deployment of embolization coils are performed from the distal to proximal direction. Sclerotherapy drugs which contain sodium tetradecyl sulfate can be used between coils to assist with treating the varicose veins.
-
Contrast injections under fluoroscopy is used to check that the left ovarian vein (single or multiple branches) are embolized and prevent contrast from travelling down towards to the pelvis. It is important to also allow some time to pass before checking to allow the coils to expand.
-
Following embolization of the left ovarian vein, the right renal vein and right ovarian vein are checked for contribution to the PCS. If PCS is demonstrated then embolization coils (and sclerosants) are used to block the right ovarian vein.
-
Following this, the left and right internal iliac veins are imaged under fluoroscopy, contrast injection, and Valsalva maneuver. If dilatation and reflux is demonstrated, then embolization coils are deployed to treat these veins.
-
The vascular devices are removed post-procedure, pressure is applied on the groin region, and the angiography table can be placed in reverse-Trendelenburg position.

Fluoroscopy (LIH) showing contrast within the pelvic varices branching off the left ovarian vein.
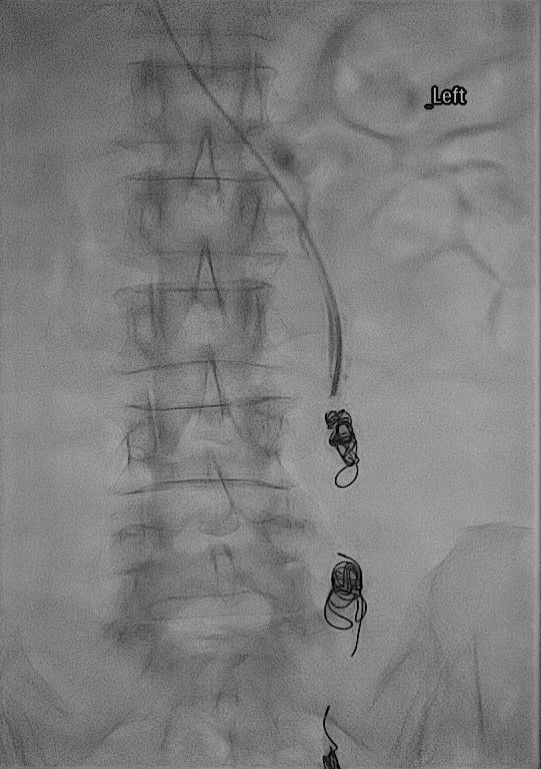
Fluoroscopy (LIH) showing contrast within the pelvic varices branching off the left ovarian vein.
-
Liu B, Yu X, Xu X, et al. Ovarian vein embolization for the treatment of pelvic congestion syndrome: a systematic review and meta-analysis. Eur Radiol. 2021;31(1):202-211. doi:10.1007/s00330-020-07245-3
-
Basile A, Vigna G, Pennisi M, et al. Ovarian vein embolization for the treatment of pelvic congestion syndrome: long-term technical and clinical outcomes. Cardiovasc Intervent Radiol. 2021;44(2):282-291. doi:10.1007/s00270-020-02634-3
-
Kim HS, Malhotra AD, Rowe PC, et al. Embolotherapy for pelvic congestion syndrome: long-term results. J Vasc Interv Radiol. 2006;17(2 Pt 1):289-297. doi:10.1097/01.RVI.0000194123.10968.10
-
Del Cura JL, García-Velasco JA, Zorrilla I, et al. Ovarian vein embolization: a new approach to the treatment of pelvic congestion syndrome. AJR Am J Roentgenol. 1998;170(6):1537-1540. doi:10.2214/ajr.170.6.9609155
-
Prologo JD, Bohnert AB, Shields JJ, et al. Imaging findings and follow-up after ovarian vein embolization for pelvic congestion syndrome. J Vasc Interv Radiol. 2015;26(9):1292-1298.e1. doi:10.1016/j.jvir.2015.04.018